A rapid, humanitarian-focused border operation unfolded in Sa Kaeo province on an early Sunday morning, as Thailand opened a permanent checkpoint to facilitate an emergency medical transfer for a high-ranking Cambodian official. The move underscored the willingness of Thai authorities to coordinate cross-border assistance even amid a sensitive political climate. The transfer highlighted the smooth cooperation between neighboring countries to address urgent health needs at the border. This article details the sequence of events, the key individuals involved, the operational considerations at the Ban Khlong Luek checkpoint, and the broader context of bilateral border management.
Timeline and the emergency transfer
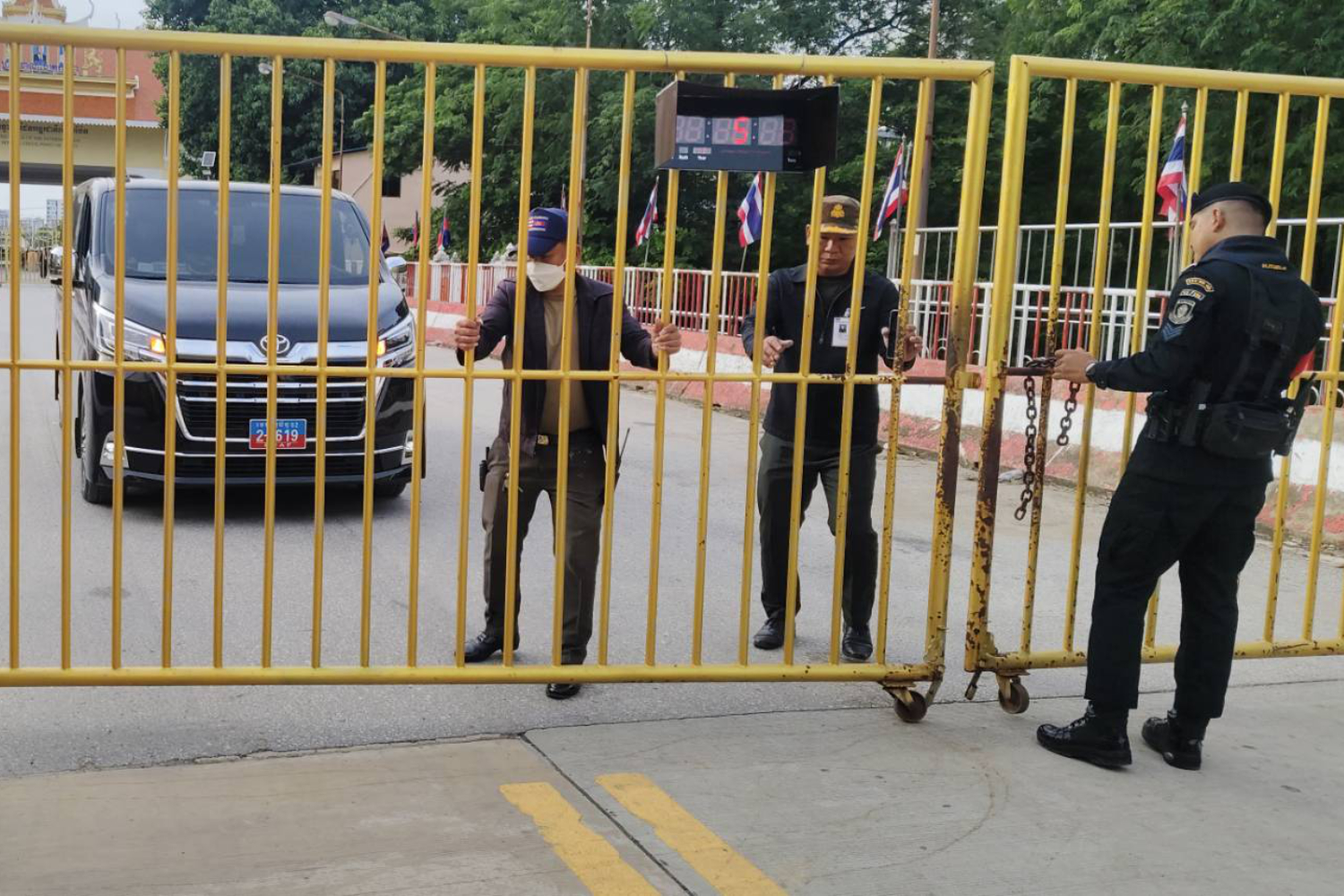
From the earliest light of day, Thai security officials activated the permanent border checkpoint at Ban Khlong Luek in Sa Kaeo province to support an urgent medical evacuation. At 7:35 in the morning, exactly as reported by the Sa Kaeo office of Radio Thailand, officials opened the border gate to permit the transfer of Lt Gen Pech Vanna. Lt Gen Pech Vanna serves as the Deputy Director-General of Cambodia’s Border Affairs Department and also heads the Cambodia-Thailand Border Coordination Office. This dual role places him at the apex of Cambodia’s cross-border border management apparatus, responsible for coordinating how Cambodia and Thailand manage shared border issues and emergencies.
The plan was to move Lt Gen Pech Vanna swiftly across the Thai-C Cambodian Friendship Bridge, a critical connection between the two nations, so that he could receive timely medical care. The destination chosen for treatment was Kasemrad International Hospital, located in the Aranyaprathet district, a facility selected for its capability to provide immediate medical attention in response to his critical condition. This transfer was undertaken with a clear emphasis on urgency, minimizing delays to ensure the patient could be stabilized and treated without impediment.
The operation occurred under the framework of a broader border management environment that sometimes experiences political and security pressures. Local authorities reported that the opening of the checkpoint for this transfer occurred within the context of bilateral border tensions that have, at times, influenced how border facilities operate. As such, the operation reflected both the humanitarian imperative to safeguard a high-ranking official’s health and the strategic concerns surrounding cross-border relations. The overall objective was to ensure a rapid, orderly transfer that respected legal, medical, and security standards while prioritizing the patient’s immediate needs.
In the immediate aftermath, the patient was transported across into Thailand to receive urgent medical care. The route, the timing, and the choice of destination hospital were all coordinated to align with the required medical interventions and the patient’s condition. The operation showcased a practical application of cross-border cooperation in the realm of health care, where life-saving transport can occur notwithstanding ongoing diplomatic sensitivities. This sequence also illustrated the capacity of border authorities to adapt operational procedures to accommodate emergencies, even when standard schedules or norms might otherwise constrain cross-border activity.
The initial report of the transfer, attributed to the Sa Kaeo office of Radio Thailand, provided a precise snapshot of the event: the border gate opened at 7:35 am, enabling the emergency crossing. The description underscored both the speed of the response and the formalities that accompany such a cross-border medical evacuation. By moving Lt Gen Pech Vanna through the Friendship Bridge to a hospital capable of delivering immediate care, Thai authorities demonstrated a commitment to rapid intervention that aligns with regional expectations for high-level cross-border health emergencies. The transfer’s successful execution depended on timely coordination among border security, health care facilities, and transportation resources.
As the patient arrived at Kasemrad International Hospital in Aranyaprathet district, medical staff there prepared to commence urgent treatment. The hospital’s readiness highlighted the importance of having capable facilities along border corridors that can accept emergency cases quickly. In border regions like Sa Kaeo and Aranyaprathet, the proximity of medical facilities to crossing points is crucial for reducing response times and improving survival odds in critical situations. The case also showcases how health systems and border control agencies collaborate to ensure that urgent care is accessible across international lines when warranted by medical necessity.
The broader significance of this operation extends beyond the immediate medical outcome. It demonstrates a functional, real-world example of how bilateral border infrastructure can be leveraged to address emergencies effectively. The Ban Khlong Luek checkpoint, described as a permanent crossing point, can thus serve not only routine trade and travel but also rapid life-saving medical evacuations when diplomatic contexts permit. The event serves as a reference point for future cross-border health interventions and for evaluating how border facilities might be optimized to handle similar emergencies with minimal disruption to normal security procedures.
In recapping the sequence, the core elements were clear: an emergency medical need, a high-ranking Cambodian official, a rapid border crossing through Ban Khlong Luek, a transfer across the Friendship Bridge, and immediate medical attention at Kasemrad International Hospital. The coordinates of the operation—7:35 am opening, the crossing, and transfer to a designated hospital—were essential for ensuring the patient received timely care while maintaining the integrity of border management protocols. The incident stands as a notable example of cross-border medical cooperation undertaken under pressure from diplomatic tensions, demonstrating that humanitarian considerations can be prioritized within the framework of international relations.
To summarize the initial portion of this timeline, the transfer was initiated at dawn, with a focus on speed and safety. The involvement of high-ranking Cambodian officials in this medical emergency underscores the seriousness of the case and the necessity for swift cross-border coordination. The border crossing at Ban Khlong Luek functioned as a conduit for urgent health care rather than solely a checkpoint for routine cross-border traffic. The operation’s outcome emphasized the ability of border authorities to adapt to extraordinary circumstances while ensuring adherence to procedural norms. The immediate result was that Lt Gen Pech Vanna received the medical attention required without unnecessary delay, at a hospital equipped to respond to critical medical situations.
In the days ahead, observers may look to the details of how this operation was managed, including the roles of border authorities, health care providers, and transportation teams. The event has implications for ongoing discussions about border infrastructure, cross-border health protocols, and the management of diplomatic sensitivities during humanitarian emergencies. While the specifics of medical treatments and patient outcomes remain private medical information, the public account confirms that a well-coordinated, cross-border response was executed to address a pressing medical need.
The key figures and institutional roles
Lt Gen Pech Vanna’s position made this case particularly significant in the context of Cambodia–Thailand border management. As Deputy Director-General of Cambodia’s Border Affairs Department and Head of the Cambodia-Thailand Border Coordination Office, he occupies a pivotal role in shaping how the two countries collaborate on border security, border management, and cross-border health interventions. His leadership responsibilities include overseeing coordination between Cambodian border authorities and their Thai counterparts, particularly in matters that affect people moving across the frontier, whether for trade, travel, or humanitarian reasons.
The transfer involved collaboration among multiple agencies and institutions to ensure the patient’s safety and rapid movement. Thai border security personnel, whose duties include monitoring and controlling entry and exit points at Ban Khlong Luek, acted to open the checkpoint for the emergency crossing. This action required precise timing and adherence to border procedures, ensuring the crossing did not compromise security while enabling lifesaving medical access across the border. In addition to border security, health authorities at Kasemrad International Hospital were responsible for receiving the patient and initiating immediate medical care, underscoring the seamless integration of border operations with the country’s health care system.
The Cambodian side’s leadership within the Border Coordination Office underscores the bilateral dimension of the operation. The decision-making and coordination that occurred under Lt Gen Pech Vanna’s leadership reflect a broader framework in which both countries manage border-related health emergencies through established protocols. The office’s existence indicates a formal structure for cross-border communication, information sharing, and cooperative responses to incidents that affect cross-border mobility and health services. This kind of institutional arrangement is designed to facilitate timely, orderly responses to emergencies, even when political tensions exist.
From a procedural perspective, the human element behind the transfer is notable. An emergency medical evacuation at an international border requires clear lines of responsibility, rapid decision-making, and effective interagency communication. The process often involves input from border control teams to clear passage for ambulances, hospital staff prepared to receive and treat the patient, and health authorities coordinating post-transfer care and potential subsequent steps. This particular operation demonstrates how those elements come together in a real-world scenario, with Lt Gen Pech Vanna’s status adding a layer of diplomatic sensitivity to the medical necessity.
We should also consider the role of the Cambodia–Thailand Border Coordination Office as a mechanism for ongoing dialogue and problem-solving at the cross-border level. Such offices are intended to facilitate smoother interactions across the frontier, helping to harmonize procedures for emergency medical cases, security clearances, and orderly border flow during urgent situations. Although the specifics of every case are unique, the general principle remains constant: when health emergencies arise at the border, there is a framework designed to enable rapid, well-coordinated responses that minimize delays and reduce risk for those involved.
In terms of capacity and readiness, Kasemrad International Hospital in Aranyaprathet District stands out as a key node in border-area healthcare delivery. Hospitals located near international borders are often selected for urgent cross-border cases due to their familiarity with emergency protocols, proximity to crossing points, and ability to provide critical care without unnecessary transport time. The hospital’s role in this event reflects a broader pattern where border-region health infrastructure is integrated into cross-border response strategies to maximize patient outcomes during emergencies.
The operation also spotlights the importance of maintaining functional, reliable border crossing points that can support civilian and official movements in urgent situations. Ban Khlong Luek’s designation as a permanent checkpoint implies ongoing readiness to address both routine traffic and extraordinary needs, such as medical evacuations. The ability to convert a routine crossing into a temporary passage for urgent medical care demonstrates the versatility of border infrastructure when coordinated with health services and diplomatic channels. This flexibility is essential for ensuring that cross-border health crises are managed effectively and ethically, with respect for both national sovereignty and international humanitarian considerations.
In this context, Lt Gen Pech Vanna’s case becomes a valuable reference for future cross-border medical emergencies. It illustrates how cross-border health interventions can be conducted with minimal disruption to normal border operations while preserving security and dignity for all parties involved. The collaboration among border officials, hospital staff, and the Cambodian border authorities sets a precedent for how similar situations might be handled going forward. Although every emergency presents its own specifics, the underlying framework—rapid decision-making, interagency cooperation, and secure, orderly passage—remains a guiding model for cross-border health responses in the region.
Border operations, tensions, and policy implications
The event occurred amid ongoing bilateral border tensions that have sometimes shaped how checkpoints operate and how crossing times are scheduled. The conduct of a cross-border medical transfer at a permanent border crossing point demonstrates the capacity of both nations to prioritize urgent humanitarian needs even when political mismatches or security concerns exist. In such circumstances, border management officials must balance security, procedural compliance, and the imperative to provide timely assistance to those in medical distress. This balance is central to maintaining trust and cooperation between neighboring states, particularly in border regions where movement across the frontier is frequent and multifaceted.
As part of the operational context, authorities indicated that the border checkpoint’s opening times were adjusted as a response to the tensions. The facility is now open from 8:00 am to 4:00 pm, a window that accommodates not only routine crossing but also the possibility of cross-border medical operations when appropriate. This adjustment underscores how border policies adapt in real time to evolving political dynamics, while still preserving the capacity to deliver essential services to those in need. It also signals to travelers and official delegations that border management remains flexible and responsive to broader regional concerns.
From a humanitarian perspective, the emergency transfer underscores a principle frequently invoked in international border policy: when lives are at stake, procedures should facilitate timely aid while maintaining accountability and order. The ability to mobilize a rapid crossing, clear passage for an ambulance, and swift hospital admission reflects the maturity of the border-management framework in handling urgent cases with due regard for safety, legality, and diplomacy. Such cases can help build goodwill and mutual confidence between neighboring countries and may influence future negotiations around cross-border health protocols and emergency response standards.
For policymakers and observers, the incident offers several implications. First, it highlights the importance of maintaining permanent, well-equipped border checkpoints that can adapt to exceptional circumstances without compromising security. Second, it demonstrates the value of an established cross-border coordination mechanism—like the Cambodia–Thailand Border Coordination Office—for streamlining response efforts during health emergencies. Third, it points to the need for clear, predefined emergency procedures that specify how officials from both sides should act when urgent medical transfers are required. Fourth, it reinforces the role of nearby medical facilities—such as Kasemrad International Hospital—as integral components of the border health ecosystem, capable of delivering urgent care promptly.
These implications also intersect with broader regional dynamics. Cross-border health interventions are intrinsically linked to the stability of border regions, economic activity, and people’s daily lives who rely on smooth movement for work, family, and access to services. In a region where communities straddle national boundaries, efficient cross-border care can reinforce social and economic ties, even when political tensions exist. By evidencing a successful cross-border medical transfer, this event may contribute to a more resilient framework for future emergencies, reassuring residents and officials on both sides that humanitarian needs can be prioritized without undermining sovereignty or security.
Operationally, security considerations remain essential. The crossing of a high-ranking official involved monitoring, verification, and maintained security protocols to prevent misuse while enabling urgent treatment. Border authorities must ensure that emergency moves follow proper authorization channels, that the information flow remains controlled, and that all actions are documented for accountability. The balance between openness for humanitarian purpose and caution against potential misuse is a constant theme in border management, particularly in fragile or tense environments. The current case indicates that this balance was achieved through careful coordination and adherence to established procedures, even under pressure.
The event also invites a closer look at the regional mechanisms that enable such cooperation. The Cambodia–Thailand Border Coordination Office serves as a focal point for aligning cross-border procedures, sharing relevant information, and coordinating joint responses to incidents that affect the border region. Its existence reinforces the importance of institutional channels that can bridge the gap between security concerns and humanitarian obligations. In a rapidly changing regional landscape, such offices may become even more critical in facilitating cooperative approaches to health, security, and migration across the frontier.
In considering the future trajectory of border policy and cross-border health interventions, several lessons emerge. The significance of maintaining ready-to-activate border health corridors is clear, as is the value of clear communication and advance planning among border agencies, health authorities, and diplomatic channels. The ability to mobilize a rapid response while upholding security and procedural standards is essential for effective border governance and regional stability. The outcome of this Sunday morning operation suggests that a well-coordinated, rights-respecting approach to emergency medical transfers across the Thai–Cambodian border can yield timely, life-saving results even amid tensions.
The broader narrative also includes the reminder that border infrastructure and health systems are deeply interconnected in ways that affect everyday life for border communities. Transportation routes, bridge crossings, and border facilities collectively support not only commerce but also access to critical care. When an emergency arises, efficient cross-border cooperation can reduce delays, improve patient outcomes, and reinforce mutual trust between neighboring nations. This event is an instructive case study in how to operationalize such cooperation under the constraints of a tense diplomatic environment, without compromising the safety and sovereignty of either country.
In summary, the immediate emergency transfer of Lt Gen Pech Vanna at Ban Khlong Luek demonstrates a functional, purpose-built response mechanism at the Thai–Cambodian border. It confirms the role of the Ban Khlong Luek checkpoint as a permanent crossing point capable of adapting to extraordinary needs. It also reinforces the importance of the Cambodia–Thailand Border Coordination Office and cross-border health facilities in sustaining rapid, coordinated action during health crises. The incident’s handling offers a constructive template for future cross-border medical evacuations and for maintaining open channels of communication and cooperation in a region where border dynamics continually evolve.
Healthcare logistics, proximity, and hospital readiness
The Kasemrad International Hospital in Aranyaprathet district was the designated destination for Lt Gen Pech Vanna’s urgent medical treatment. In border regions, such facilities play a crucial role in bridging the gap between immediate border response and definitive medical care. Their proximity to international crossings allows for rapid transfer times, reducing the window during which a patient’s condition could deteriorate. The hospital’s readiness for such a transfer reflects the health system’s capacity to handle high-priority emergencies that come with cross-border movement and international routes.
From a logistics standpoint, the medical team at Kasemrad International Hospital would have coordinated with border authorities to receive the patient in a secure, controlled manner. The hospital would need to allocate critical care resources, such as emergency physicians, nurses, intensive care capabilities if needed, and imaging or diagnostic services essential to the patient’s condition. The speed of transfer, combined with the hospital’s readiness to deliver immediate care, is a cornerstone of the successful management of cross-border medical emergencies. The ability to respond quickly reduces the risk of complications and increases the likelihood of positive health outcomes for high-priority patients.
The episode also underscores the importance of having a formalized process for cross-border medical transfers. Establishing protocols for fast-track admission, patient handover, and information sharing between border security teams and hospital staff is essential for ensuring smooth operations. Such protocols may include standardized documentation, rapid verification procedures, and pre-notification to receiving facilities to prepare for immediate treatment upon arrival. The efficiency of these steps can directly influence the patient’s prognosis, especially in cases involving life-threatening or time-sensitive conditions.
In terms of patient safety and privacy, medical teams handling cross-border transfers must adhere to applicable medical ethics and data protection standards. While the specifics of Lt Gen Pech Vanna’s medical condition are not publicly disclosed, the overarching principle remains that patient care should be delivered with professionalism, discretion, and respect for patient privacy. The hospital’s care team would balance the urgency of treatment with the need to protect sensitive health information, ensuring that only authorized personnel have access to medical data. The coordination among border authorities and hospital staff likewise respects legal and ethical boundaries.
The logistical success of this transfer also highlights the value of well-maintained transport infrastructure along border corridors. The Thai-Cambodian Friendship Bridge provides a critical route for quick passage between the two countries, enabling not only person-to-person travel but also efficient medical evacuations. The presence of a reliable bridge connection reduces travel time for ambulances and medical teams, ensuring the patient can reach a facility capable of providing definitive care in a timely manner. Bridge infrastructure thus becomes a vital component of border resilience, particularly in emergencies where every minute counts.
Additionally, the operation reflects on the broader healthcare system’s capacity in border towns to absorb urgent cases from neighboring countries. The case demonstrates that cross-border health collaborations can extend the reach of medical services beyond national borders, particularly when urgent care is necessary and when a patient’s condition requires immediate intervention. This reality may influence how regional health networks plan for cross-border health needs, including the allocation of resources, training for border health responders, and coordination with international health authorities.
In the context of Sa Kaeo province and its border area, the event likely involved a network of local health authorities, hospital administrators, and border security units working together to ensure a seamless transition from border crossing to hospital admission. Such cooperation requires clarity of roles, efficient communication channels, and shared understanding of the patient’s medical priorities. The ability to deliver urgent care across borders reinforces the value of integrated regional health services that can respond to emergencies across national boundaries when warranted by medical necessity.
The hospital’s role in this scenario also highlights the importance of having cross-border health agreements and mutual aid arrangements. While the specifics of any formal agreement are not described in the available account, the practical outcome—swift admission and initiation of treatment—suggests that mechanisms exist to support cross-border health transfers. These arrangements may be part of a broader framework designed to facilitate humanitarian responses, expand cross-border health care, and strengthen regional resilience in the face of medical emergencies that cross national lines.
Finally, from a public health perspective, incidents like this can contribute to strengthening regional preparedness for medical emergencies. They provide real-world data on the efficacy of cross-border transfer protocols, hospital readiness, and the coordination between border authorities and health care providers. By examining how this transfer was executed, health officials across the region can identify best practices and potential areas for improvement in cross-border emergency response, emergency medical services, and hospital throughput. The ongoing refinement of these processes is essential to ensure that future incidents receive similarly rapid and effective medical attention, regardless of the political climate or border tensions that may exist at any given time.
Implications for regional relations and border governance
The Sunday morning medical transfer demonstrates how cross-border border governance, health services, and diplomatic relations intersect in practical terms. It offers a model of how nations can collaborate in urgent, life-saving actions while continuing to address broader concerns in their bilateral relationship. The event reinforces the idea that humanitarian needs can take precedence in the execution of border policy, provided that appropriate security, legal, and procedural safeguards are observed. In this sense, border governance can adapt to respond to emergencies without setting a precedent that erodes the integrity of security protocols or national sovereignty.
This case also contributes to ongoing discussions about how border infrastructures and cross-border health systems can be integrated more effectively. The Ban Khlong Luek checkpoint’s status as a permanent facility, coupled with a clear, operational path for emergency medical transfers, demonstrates a level of readiness that can reassure both residents near the border and officials who manage cross-border relations. It underscores the value of maintaining functional communications channels between border agencies and health authorities on both sides of the frontier. Such channels help ensure that cross-border medical needs are met quickly and safely, even when diplomatic tensions are present.
From a regional security and diplomacy perspective, the incident illustrates the importance of balancing assertive border management with humanitarian channels. The ability to facilitate an emergency medical transfer through a high-security border crossing while maintaining orderly, documented procedures signals a mature approach to border governance in a sensitive region. It also suggests that cross-border exchanges—whether for health, trade, or diplomacy—can be conducted with professionalism and respect for the bilateral relationship. In this sense, the event can be seen as a constructive demonstration of how neighboring countries can cooperate for the common good, even when tensions exist in other areas of policy or diplomacy.
The involvement of Lt Gen Pech Vanna in this operation adds a diplomatic dimension to the narrative. As Deputy Director-General of Cambodia’s Border Affairs Department and Leader of the Cambodia–Thailand Border Coordination Office, his participation underscores the primacy of cross-border coordination in ensuring that urgent health needs are addressed with legitimacy and transparency. The incident highlights the importance of having senior representatives and official coordination mechanisms to oversee cross-border health responses, ensuring that actions taken at the border align with both countries’ policies and international norms.
In terms of policy development, the event provides a real-world case for evaluating and potentially enhancing cross-border health protocols. Policymakers can examine how emergency health transfers are executed, what improvements could reduce response times further, and how to harmonize hospital intake procedures with border entry processes. The case also suggests opportunities to refine the hours of operation for permanent border checkpoints to accommodate emergencies more consistently, while still safeguarding security considerations. Future policy discussions might explore the feasibility of expanding emergency transfer windows or implementing dedicated lanes for medical evacuations at strategic border crossings.
The cross-border dimension of this event is particularly relevant for regional governance strategies that aim to strengthen resilience in border areas. Healthcare collaboration, coordinated border management, and reliable transport corridors are essential components of a robust regional security framework. The successful emergency transfer through Ban Khlong Luek adds a tangible example to the broader discourse on how neighboring countries can work together more effectively to support vulnerable populations and high-ranking officials alike during critical moments. It demonstrates that, even amid tensions, the shared interest in protecting life and health can drive cooperative solutions that benefit both sides.
Looking ahead, the incident may encourage ongoing dialogues about emergency response protocols, joint training exercises for border authorities and health workers, and the development of standardized procedures for high-priority medical evacuations. Such initiatives could further streamline cross-border health transfers, reduce potential delays, and enhance accountability. By fostering continuous improvement in border governance and cross-border health collaboration, the region can build a more reliable, humane, and efficient system for responding to urgent medical needs across borders in the future.
Projections for border policy and cross-border health care
TheSunday morning operation is likely to influence future practice in cross-border health initiatives and border management across the Thai–Cambodian frontier. Given the demonstrated capability to accommodate an emergency medical transfer at a permanent border crossing, policymakers may consider formalizing more robust cross-border health protocols, including clearer criteria for medical evacuation eligibility, standardized patient handover procedures, and mutual recognition of hospital readiness across the border. The integration of health services with border security processes can be optimized to ensure that urgent care is delivered promptly without compromising security and sovereignty.
A potential area of focus could be the expansion of dedicated medical transfer routes within border crossings that frequently handle urgent cases. This could involve the designation of priority lanes for ambulances during emergencies, pre-cleared entry flags for medical teams, and real-time coordination platforms that connect border authorities with receiving hospitals. By implementing such enhancements, border regions could maintain high security while maximizing the speed and efficiency of cross-border medical interventions. This would be particularly valuable in scenarios involving senior or high-profile officials, where bureaucratic delays could have significant health implications.
Another aspect worth addressing is the ongoing management of border opening hours in response to occasional spikes in tensions. The current adjustment to an 8:00 am–4:00 pm window may be revisited as part of a broader review of border operational policies. A structured approach to evaluating daily crossing needs, humanitarian exceptions, and emergency scenarios could help determine whether more flexible hours are warranted, and under what conditions such flexibility would be applied. Any changes would need to balance security considerations with humanitarian priorities, ensuring that cross-border cooperation remains predictable, transparent, and accountable.
The event also reinforces the value of continuous training and exercises for border and health authorities. Regular joint drills that simulate cross-border medical evacuations would help identify bottlenecks and enable teams to refine procedures. Such exercises could cover various scenarios, including different times of day, weather conditions, and the involvement of multiple agencies. The objective would be to build a resilient, practiced response framework that can be deployed rapidly whenever emergencies arise, thereby reducing the risk of delays and improving patient outcomes.
Beyond procedural improvements, there is a broader imperative to strengthen regional trust and collaboration. Cross-border health incidents, when managed effectively, can reinforce diplomatic ties and foster mutual confidence between neighboring nations. The narrative surrounding the Lt Gen Pech Vanna transfer may contribute to a broader sentiment of cooperation and shared responsibility for humanitarian outcomes. Over time, this can translate into increased regional stability, more cooperative border governance, and improved infrastructure for cross-border health care, all of which benefit communities living near the frontier.
In the long term, the Thai–Cambodian border could become a model for how nations address cross-border emergencies with care, accountability, and efficiency. By maintaining well-equipped border crossings, strengthening coordination offices, and investing in border-region health facilities, both countries can ensure that urgent medical needs are met swiftly and safely, even in periods of tension. The lessons learned from this operation may inform policy and practice across other border areas in Southeast Asia, contributing to a more resilient, cooperative regional landscape where humanitarian concerns are prioritized alongside national security and sovereignty.
Conclusion
The emergency medical transfer of Lt Gen Pech Vanna across the Thai–Cambodian border at Ban Khlong Luek highlights the operational capacity of permanent border checkpoints to support urgent humanitarian needs. The sequence—opening of the border gate, rapid cross-border passage via the Friendship Bridge, and immediate medical care at Kasemrad International Hospital—illustrates a coordinated effort among border security, health care providers, and cross-border authorities. The involvement of Lt Gen Pech Vanna, a senior Cambodian official responsible for border affairs, adds significance to the event, underscoring the importance of cross-border cooperation at the highest levels of government.
The operation occurred against a backdrop of bilateral border tensions, which led to adjustments in the checkpoint’s opening hours, now set from 8:00 am to 4:00 pm. This adjustment demonstrates the dynamic nature of border governance, where security considerations and humanitarian needs must be balanced with diplomatic realities. Despite the tensions, the successful transfer showed that cross-border collaboration remains a practical, achievable objective when there is a clear framework for coordination and a shared commitment to saving lives.
The incident also reinforces the critical role of the Cambodia–Thailand Border Coordination Office and the surrounding health infrastructure in enabling rapid responses to cross-border medical emergencies. It provides a pragmatic blueprint for how border regions can be prepared to handle urgent health events, ensuring that high-priority patients receive timely treatment while maintaining border security and procedural integrity. As the region continues to navigate a complex political landscape, such examples of cooperative action can contribute to more resilient, humane border governance and stronger regional ties.